Home » Risk Adjustment
An AI-powered platform that seamlessly bridges patients and care teams, enhancing Communication and engagement are essential for success in value-based care models to support better health outcomes and reduce costs.
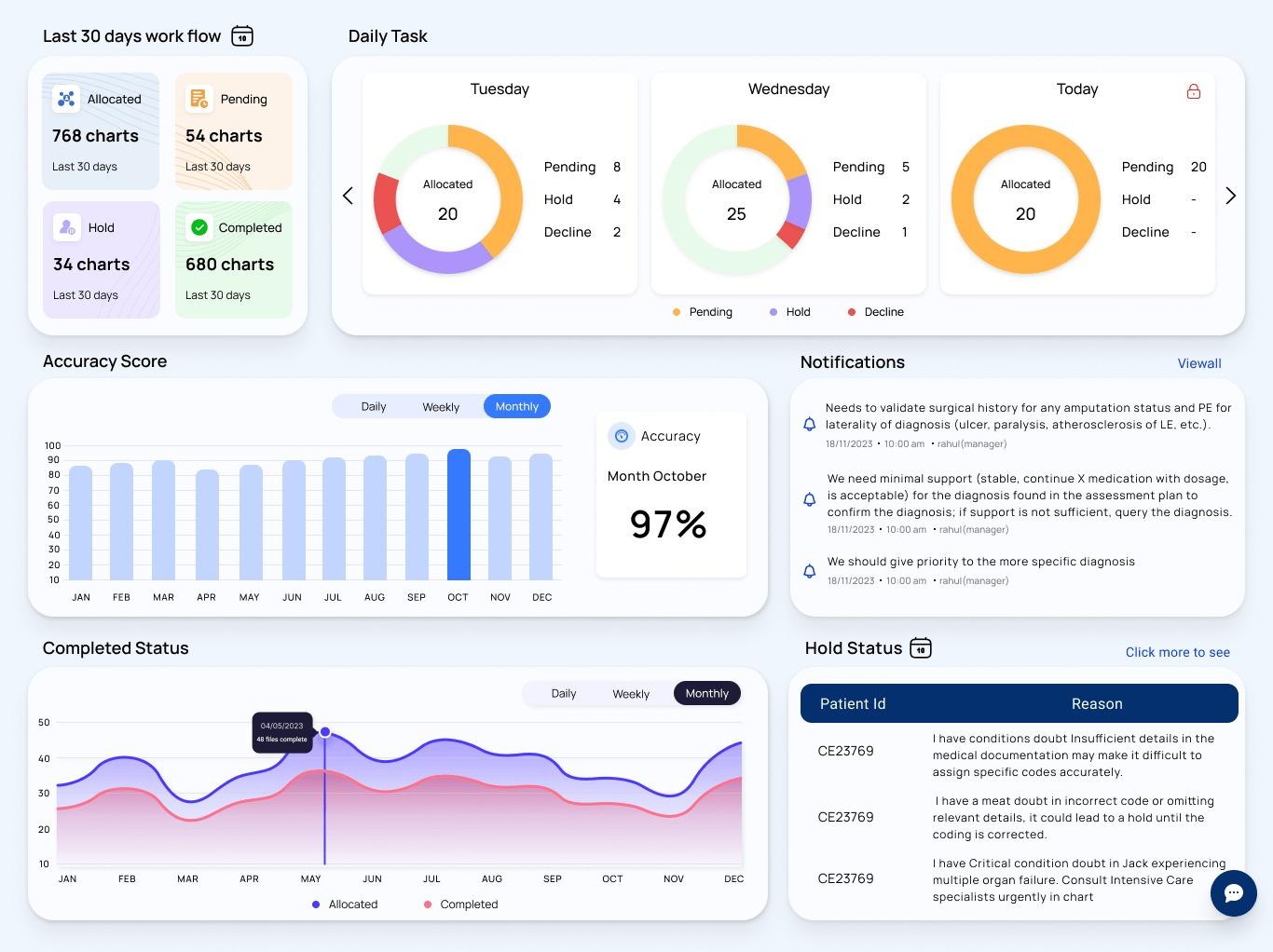
Monitor and forecast claim issues, DRG shifts, and denial risks with live dashboards and AI-powered insights enabling faster, data-driven decisions.
Automatically validate ICD-10, PCS, and DRG assignments against clinical documentation to ensure accuracy and compliance before billing.
GenAI detects documentation gaps and generates compliant, physician-ready queries to improve specificity, reduce rework, and enhance RAF scores.
Assign each record a denial risk score based on historical trends, documentation quality, and coding patterns, empowering teams to act proactively.
Unlock smarter, faster, and more accurate risk adjustment workflows with Alpine Pro Health’s GenAI-enabled solution. Whether you’re conducting retrospective, prospective, or concurrent reviews, our intelligent platform streamlines the process with precision. Designed to elevate coding accuracy and transform clinical data into actionable insights, this solution empowers healthcare organizations to stay compliant, improve RAF scores, and drive better outcomes through automation and data intelligence.
Utilizes NLP and machine learning to extract and assign accurate HCC codes directly from clinical notes.
Automatically updates RAF scores as diagnoses are coded, providing real-time visibility into patient risk and reimbursement impact.
Identifies missed or unsupported diagnoses and flags documentation gaps to prevent revenue leakage.
Verifies that each HCC is fully supported by clinical evidence, ensuring readiness for RADV and payer audits.

Enhanced Accuracy with
AI & Clinical Intelligence
Built-In Audit Readiness
and Compliance
Faster Turnaround Times and
Optimized Revenue
Established in 2022, Alpine Pro Health. delivers accurate, compliant, and efficient medical coding and RCM solutions. Trusted by U.S. healthcare providers for expert-driven, end-to-end services.
131 Continental Dr, Suite 305, City of Newark, County of New Castle, Delaware 19713.
97, 98, Level 1, Magna Square, Jawaharlal Nehru Rd, Ashok Nagar, Chennai, Tamil Nadu, 600083, India
All Rights Reserved © 2025 Alpine Pro Health